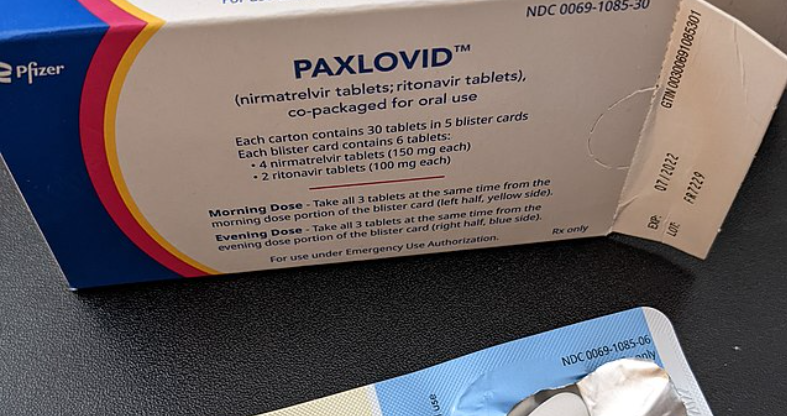
According to new research, there is no reduction in Long COVID risk with the use of Paxlovid.
Others are reading now
In a pivotal study, researchers have discovered that Paxlovid, a medication used for treating COVID-19, does not reduce the risk of developing long COVID symptoms. The study, published in the Journal of Medical Virology, found that 16.1% of patients treated with Paxlovid reported long COVID symptoms, which is only marginally lower than the 14% in untreated patients.
Long COVID, a condition affecting approximately 10% of COVID-19 patients globally, manifests in a variety of symptoms, such as chest pain, nausea, fatigue, and cognitive impairment. While previous studies indicated that vaccination could reduce the risk of long COVID, it doesn’t eliminate the risk entirely.
The study, led by investigators from the University of California San Francisco Medical Center, was an observational cohort study. It included participants who were vaccinated against COVID-19, not hospitalized, not pregnant, and tested positive for SARS-CoV-2 between March and April 2022. Of these, 988 were treated with Paxlovid and 3696 were not. A survey was conducted to assess long COVID symptoms among these participants.
Also read
Fatigue, Confusion, Headache
Results showed that the most commonly reported long COVID symptoms among those treated with Paxlovid were fatigue, shortness of breath, confusion, headache, and altered taste and smell. The findings were consistent even when variables like demographics, medical history, and substance use were taken into account. In Paxlovid-treated patients who reported at least one long COVID symptom, the median number of symptoms was one, compared to two in untreated patients.
Study limitations included a relatively homogenous cohort, reliance on self-reports, the survey not encompassing all long COVID symptoms, and the inclusion of objectively measured post-COVID outcomes.
Matthew Durstenfeld, the lead author of the study, noted a higher proportion of clinical rebound than previously reported but found no effect of post-treatment rebound on long COVID symptoms. He expressed surprise that Paxlovid treatment during acute infection was not associated with lower odds of long COVID, a finding consistent with other studies that also found no difference in post-COVID conditions between four and six months after infection